Crucial Vitamins & Minerals

Multivitamins
Your doctor or nurse midwife may have recommended that you take a prenatal multivitamin containing the recommended amounts of vitamins, including folic acid. Your prenatal vitamin is very important throughout pregnancy to support the growth of the baby and maintain your health. Be sure to take it every day.
Important note: Vitamins do not take the place of good eating. Talk to your doctor or nurse-midwife before taking any vitamin or herbal-supplement. Never take a supplement that contains more than the Daily Value (DV) of vitamins and minerals without talking to your doctor or nurse midwife, because large doses of certain vitamins (such as vitamin A) may harm your baby.
Folic acid
Pregnant women need 400 micrograms (400mcg) of folic acid every day to help prevent birth defects. Folic acid is important for any woman who could possibly become pregnant. Folic acid is a B vitamin that helps prevent serious birth defects of a baby's brain or spine called neural tube defects. Adequate amounts can decrease the risk of neural tube defects by 50-70%. Getting enough folic acid can also help prevent birth defects like cleft lip and congenital heart disease.
Folic acid is most important very early in pregnancy, usually before a woman knows she is pregnant. If you are of childbearing years it is suggested that you maintain an adequate amount in your diet or by supplementation. At least one month before you try to become pregnant, or once you become pregnant, you should make sure you're getting enough folic acid. Most multivitamins sold in the U.S. contain enough folic acid for the day. Many prenatal vitamins contain up to 1000 mcg (1mg) of folic acid. Be sure to check the label. Choose a multivitamin that contains at least 400 mcg or 100% of the Daily Value (DV) for folic acid. Eating a serving of fortified breakfast cereal will also provide 100% DV of folic acid.
Dietary Sources of Folate (Folic Acid)
| Food | Serving | Folate Micrograms |
|---|---|---|
| Brewer's Yeast | 1 tablespoon | 313mcg |
| Blackeyed Peas | 1/2 cup cooked | 280mcg |
| Lentils | 1/2 cup cooked | 180mcg |
| Turnip Greens | 1 cup | 171mcg |
| Lima Beans | 1 cup cooked | 137mcg |
| Orange Juice | 8 ounces | 136mcg |
| Kidney Beans | 1/2 cooked | 115mcg |
| Romaine Lettuce | 1 cup | 100mcg |
| Broccoli, raw | 1 cup | 62mcg |
| Bok Choy, raw | 1 cup | 57mcg |
Folate
Low folate levels are linked to birth defects like spina bifida, because folate is required for protein-tissue construction. Eating foods that contain folic acid (orange juice, leafy-green vegetables and fortified breakfast cereals) is helpful. Even when taken before pregnancy - and within the first 6-weeks of pregnancy - adequate amounts of folic acid may help reduce the risk of birth defects of the brain and spinal cord.
Important note: Vitamins do not take the place of good eating.
Iron
Pregnant women need twice as much iron as non-pregnant women, 30 mg per day. The Centers for Disease Control and Prevention (CDC) recommends that pregnant women start taking a low-dose iron supplement (30 mg/day) or a multivitamin with iron beginning at the time of their first prenatal visit. Ask your doctor or nurse midwife what he or she recommends. Prenatal vitamins prescribed by your doctor or those you can buy over-the-counter usually have the amount of iron you need. Always read the label to make sure. Pregnant women should also eat iron-rich foods. Some good dietary sources of iron include lean red meat, fish, poultry, beans, dried fruits, dark leafy greens, whole grain breads, and iron-fortified cereals. Pregnant women need extra iron for the increased amount of blood in their bodies and to help deliver oxygen across the placenta to baby. Your baby also needs to store iron in his body for the first few months of life. Too little iron can cause a condition called anemia. If you have anemia, you might look pale and feel very tired. Your doctor will check for signs of anemia in the routine blood tests taken at the different stages of your pregnancy. If your doctor finds that you have anemia, she may recommend a special iron supplement to take once or twice a day.
Dietary Sources of Iron
| Food | Serving | Iron Milligrams |
|---|---|---|
| Tofu | 1/2 cup | 6.7mg |
| Black Strap Molasses | 1 tablespoon | 5mg |
| Lentils | 1/2 cup cooked | 3.3mg |
| Beef | 3 ounces | 2/8-3mg |
| Lima Beans | 1/2 cup cooked | 2.9mg |
| Soy Beans | 1/2 cup cooked | 2.5mg |
| Kidney Beans | 1/2 cup cooked | 2.2mg |
| Turkey | 3 ounces | 2mg |
| Kale | 1 cup cooked | 1.8mg |
| Pumpkin Seeds | 2 tablespoons | 1.8mg |
| Spinach, raw | 1 cup | 1.7mg |
| Broccoli, raw | 1/2 cup | 1.7mg |
| Almonds | 1/4 cup | 1.6mg |
| Tuna | 3 ounces | 1.6mg |
| Peas | 1/2 cup cooked | 1.5mg |
| Collard greens | 1 cup cooked | 1.5mg |
Calcium
Pregnant women aged 19 to 50 years should get 1,200 mg/day of calcium through diet or supplementation. Younger pregnant women may need even more calcium, up to 1300 mg/day. Most women in the U.S. don't eat enough calcium. During your pregnancy, you may have to change your diet to get enough of this important mineral. Low-fat or non-fat milk, yogurt, cheese or other dairy products are great sources of calcium. Eating green leafy vegetables and calcium-fortified foods like orange juice and breakfast cereal can also provide calcium. If your diet is not providing 1,200 mg/day of calcium, talk to your doctor about taking a calcium supplement.
Dietary Sources of Calcium
| Food | Serving | Calcium Milligrams |
|---|---|---|
| Cheese | 3 ounces | 500-800mg |
| Sardines, with bones | 3 ounces | 372mg |
| Collard Greens | 1 cup cooked | 357mg |
| Yogurt | 8 ounces | 345mg |
| Milk | 8 ounces | 300mg |
| Spinach | 1 cup cooked | 276mg |
| Oatmeal, fortified | 1 cup cooked | 208mg |
| Tofu | 6 ounces | 190mg |
| Broccoli | 1 cup cooked | 180mg |
| Soy Milk, fortified | 8 ounces | 167mg |
| Cottage Cheese | 8 ounces | 155mg |
| Swiss chard | 1 cup cooked | 138mg |
Fiber
A high fiber diet can help prevent constipation and hemorrhoids. Certain types of fiber also slow absorption of glucose and increase insulin sensitivity, and therefore assist in healthy blood sugar maintenance. Adequate fiber intake may help decrease risk for hypoglycemia, morning sickness, and gestational diabetes. You should eat at least 25 grams of fiber each day. Eat a well-balanced diet that includes lots of fresh fruits and vegetables, whole grain breads and cereals, and unprocessed bran.
| Food | One Serving | Food | One Serving |
|---|---|---|---|
| Apple | 1/2 | Mustard greens | 1 cup |
| Apricots | 3 | Nectarine or peach (raw) | 1 medium |
| Banana | 1/4 | Small peanuts | 20 |
| Beets (cooked) | 1/2 cup | Pear (raw) | 1/2 medium |
| Broccoli (cooked) | 1/3 cup | Peas (raw) | 1/6 cup |
| Brown rice (cooked) | 1 cup | Popped Popcorn | 2 cups |
| Cantaloupe | 1.25 cup | Potato (baked) | 1/2 cup |
| Carrots (cooked) | 1/2 cup | Spinach (cooked) | 1/6 cup |
| Cauliflower (cooked) | 2/3 up | Sweet corn (cooked) | 1/4 cup |
| Cherries | 20 | Large Watermelon | 1.5 cups |
| Cucumber | 1 cup | Whole grain bread | 1 slice |
| Green beans (raw) | 1/4 cup | Whole wheat crackers | 6 |
| Green pepper (raw) | 1 cup | Zucchini (raw) | 1/2 cup |
| Honeydew melon | 1.5 cups |
Foods with 8 Grams of Fiber per Serving
| Food | One Serving |
|---|---|
| All Bran | 1 cup |
| Bran Chex® or Corn Bran® | 1 cup |
| Brown, kidney, lima, pinto or white beans | 1/2 cup |
| Grapenuts® | 9 tablespoons |
| Lentils (cooked) | 1 cup |
| Shredded Wheat® | 3 biscuits |
Healthy Foods and the Food Guide Pyramid
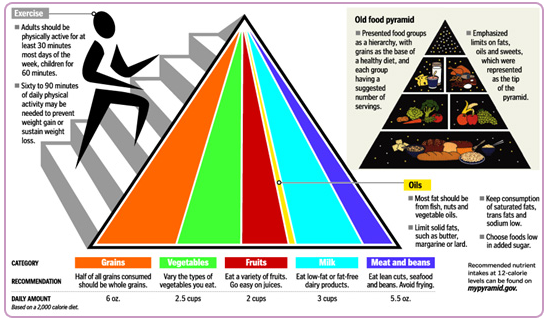
A pregnancy diet must provide both mom and developing baby with the necessary amounts of protein, carbohydrates, fats, fiber, vitamins, and minerals. A balanced diet includes eating from each of the food groups every day.
Visit www.choosemyplate.gov to learn more!
Also check out the article - Healthy Diet & Lifestyle, Food Groups, Nutrition Before & During Pregnancy, Child Nutrition, Physical Activity by Meghan Lambert.
Fats, Oils, and Sweets
The Food Guide Pyramid suggests eating fats, oils, and sweets sparingly. These foods should be the smallest percentage of your diet. Often these foods are high in calories and low in other nutrients, or "nutrient-poor". It is important to fill your diet during pregnancy with "nutrient-dense" foods such as those discussed above. When eating from this food group, choose a minimal amount of healthy fats such as nuts and avocadoes, healthy oils such as olive, flax, or sesame, and natural sweets such as whole fruits. Try to eliminate trans-fatty acids and partially hydrogenated oils. Unfortunately, the Food Guide Pyramid does not take into account the need for oils such as essential fatty acids (Omega 3 and 6). Nuts and seeds are food sources of essential fatty acids and fish provides DHA, an essential Omega 3 important for the development of your baby.
Vitamin K
Vitamin K is important in the process of blood clotting. Vitamin K does not transport well across the placenta. Decreased levels in newborns have been associated with hemorrhagic disease. Your doctor or nurse-midwife may offer your baby an injection of Vitamin K at birth, but you can get a head start by including Vitamin K rich foods in your diet. Some sources indicate Vitamin K intake should be from 65-140mcg daily during pregnancy, but an optimal intake amount may be as high as 750mcg daily.
| Food | Serving | Vitamin K Micrograms |
|---|---|---|
| Turnip Greens | 1/2 cup cooked | 471mcg |
| Broccoli | 1 cup cooked | 360mcg |
| Cabbage | 1/2 cup cooked | 91mcg |
| Spinach | 1 cup cooked | 49mcg |
| Asparagus | 4 stalks | 34mcg |
| Oats | 1 cup cooked | 30mcg |
Essential Fatty Acids (Healthy Oils)
Research over the last 30 years has indicated the importance of Omega 3 essential fatty acids, especially DHA, in the growth and development of the fetal and infant nervous system, brain, eyes and immune system. "Essential" means that these particular fats (or oils) are not produced by our bodies and must be obtained through our diet. More recent studies suggest a correlation between low levels of Omega 3 oils and DHA with attention issues and post-partum depression. Higher levels of maternal DHA during pregnancy have also been correlated with higher IQ in the children of these mothers. Alpha-linolenic acid (ALA) is the upstream Omega 3, meaning that your body must convert ALA to DHA through various biochemical steps. ALA is found naturally in flax seeds, walnuts and many other seeds and nuts. Unfortunately, some individuals may not convert ALA to DHA appropriately. DHA is found in human breast milk and fish. Although important to eat small amounts of fish during pregnancy, issues with contamination by heavy metals like mercury and toxins such as PCBs, leave us with very few dietary alternatives to supply DHA directly. You may wish to speak with your doctor or nurse midwife regarding a quality fish oil supplement. Always check that the manufacturer has tested their products for contaminants and that the product does not contain excess Vitamin A or D.
More is Not Always Better
Certain nutrients have an established upper intake level that is considered safe during pregnancy. In pregnant women ages 19-50, you should not exceed the daily amount listed below unless prescribed by your doctor or nurse-midwife. Upper intake levels include what you are receiving from both diet and supplements. Know the difference between water-soluble and fat-soluble vitamins, Watersoluble vitamins like the B vitamins and Vitamin C are utilized upon intake and excess doses are flushed from your body and do not accumulate. Fat-soluble vitamins like Vitamins A, D, E and K are stored in your liver and excess amounts can accumulate in you or your baby which may lead to toxicity or birth defects.
Vitamins
Vitamin A: 5000IU/day This amount refers only to preformed Vitamin A (retinol) and not to beta-carotene precursors. Many vegetables and multivitamins provide the precursors, or carotenes, which are water-soluble and safe during pregnancy. These precursors are changed to Vitamin A by your liver as your body requires. According to the American College of Obstetrics and Gynecology, women should also discontinue use of retinol based acne medications before and during pregnancy.
- Vitamin D: 50mcg/day or 2000IU/day
- Vitamin E: 1000mcg/day or 1500IU/day
- Vitamin C: 2000mg/day
- Vitamin B6: 100mg/day
- Niacin: 35mg/day
- Folate (Folic Acid): 1000mcg/day
- Choline: 3500mg/day
Minerals
- Sodium: 2300mg/day
- Chloride: 3600mg/day
- Calcium: 2500mg/day
- Phosphorus: 3500mg/day
- Magnesium: 350mg/day
- Iron: 45mg/day
More About Nutrition
Food Safety

Content Provided by March of Dimes
What you need to know:
Not all foods are safe for pregnant women. Some contain high levels of chemicals that can affect your baby's development. Others put you at risk for getting an infection that can hurt your baby.
What you can do:
Use common sense when preparing and selecting foods. Avoid the following:
- Swordfish, shark, king mackerel and tile fish. These fish can contain potentially risky levels of mercury. Mercury can be transferred to the growing fetus and cause serious health problems. Also avoid game fish until you check its safety with your local health department. (A game fish is any fish caught for sport, such as trout, salmon or bass.)
- Raw fish, especially shellfish (oysters, clams)
- Undercooked meat, poultry and seafood. Cook all of them thoroughly to kill bacteria.
- Do not eat hot dogs or luncheon meats. Examples are deli meats such as ham, turkey, salami and bologna. If you do eat these foods, reheat them until steaming hot.
- Refrigerated pates or meat spreads. Canned versions are safe.
- Refrigerated smoked seafood unless it has been cooked (as in a casserole). Canned versions are safe.
- Soft-scrambled eggs and all foods made with raw or lightly cooked eggs
- Soft cheeses made with unpasteurized milk. Examples are Brie, feta, Camembert, Roquefort, blue-veined, queso blanco, queso fresco and Panela. Check the label to see what kind of milk was used to make the cheese.
- Unpasteurized milk and any foods made from it
- Unpasteurized juices
- Raw vegetable sprouts, including alfalfa, clover, radish and mung bean
- Herbal supplements and teas
Also do not eat too much liver. It contains high amounts of vitamin A, which can lead to birth defects.
Some studies indicate that your baby may be at increased risk of developing a food allergy in later life if you, your partner or a family member has a food allergy. You may wish to consult a food allergy specialist for help in planning your diet during pregnancy and breastfeeding.
Drink Plenty of Water
Pregnant women should drink at least 6-8 eight-ounce glasses of water per day plus another glass of water for each hour of activity. Water plays a key role in your diet during pregnancy. It carries the nutrients from the food you eat to your baby. It also helps prevent constipation, hemorrhoids, excessive swelling, and urinary tract or bladder infections. Drinking enough water, especially in your last trimester, prevents you from becoming dehydrated. Not getting enough water can lead to dizziness, decreased blood pressure, and premature or early labor. Minimize juice and caffeinated beverages. Juices provide water, but can also be high in calories and sugar. Coffee, soft drinks, and black or green teas with caffeine may reduce the amount of fluid in your body.
A Few Healthy Pregnancy Snacks
- fresh fruit dipped in yogurt
- vegetables and dip (preferably spinach or dill)
- hummus and whole grain pita
- pretzels or popcorn (light salt and butter)
- nuts (raw are better than roasted and salted)
- frozen bananas rolled in granola
- cheese and whole grain crackers
- nut butter on rice cakes
- boiled egg
- dried fruit, unsweetened
- fresh vegetable or fruit juice made in a juicer

Food Cravings
Why do we crave foods during pregnancy? This is an as yet unanswered question. One theory is that our cravings are indicative of a nutrient required by our body. Certain food cravings may be a message from our body. For example, chocolate is high in magnesium, ice cream high in protein and calcium, meat high in protein and iron, citrus fruits and strawberries are high in Vitamin C. Cravings are natural during this phase of your development. If you want a big, juicy cheeseburger or a pint of ice cream, then have one! Or you may want to try a healthier choice that provides similar nutrients. Just be certain not to replace healthy foods with unhealthy foods.
Important Note: If you begin craving foods that aren't foods, please call your doctor or nurse midwife. Pica is a condition where you crave or eat non-food items such as dirt, paint, or paste. This condition is associated with mineral deficiencies such as iron, calcium, or zinc.

Vegetarian and Vegan Moms
If you are a vegetarian or vegan mom, you will have some special considerations during pregnancy. All vegetarians must be careful to maintain adequate intakes of protein as they are not consuming some of the main protein sources such as meat, poultry, and fish. Vegans also do not consume dairy and egg products. Vegans must be especially careful to get adequate amounts of not only protein, but also Vitamin B12 which is only available from animal products. Calcium can be consumed in dark leafy green vegetables, or supplements. Vegetarians or vegans may not convert adequate EPA and DHA from alpha-linolenic acid found in nuts and seeds, and may want to consider a fish oil product that is high in DHA. Vegetarian and vegan moms should pay special attention to consuming tofu and soy products, beans, nuts and seeds, sea vegetables, and dark, leafy green vegetables along with their normal variety of healthy food choices.
 PREGNANCY
PREGNANCY  GIVING BIRTH
GIVING BIRTH  BABY CARE
BABY CARE  HEALTH & SAFETY
HEALTH & SAFETY  FUN STUFF
FUN STUFF  FAMILY
FAMILY 